Home » Treatments » Orthodontics / Orthognatic Surgery
What is orthodontics and who can promote orthodontic care?
Orthodontics is one of the recognized specialties by the Portuguese Dental Association (OMD), which purpose is to correct the positions of the teeth in the dental arches and to move the jaws into a more balanced position.
The main purpose of orthodontics is to allow an aesthetic harmonization of the face and teeth and achieve adequate functionality of the oral structures.
Due to its specificity and according to the adopted norms in most countries, the practice of this specialty requires knowledge granted by a post-graduate training in the orthodontic area after concluding the Dental Medicine degree.
Legally, the title of specialist in orthodontics is obtained after public exam in the Portuguese Dental Association (OMD), which can only be required after successful training in a postgraduate course in this area of knowledge in a university department or national/foreigner higher education unit, with a minimum length of 3 years part-time or 2 years full-time. Only dental practitioners who attain the specialist title through the Portuguese Dental Association are authorized to publicly use the title of orthodontist.
An orthodontist is a specialized dentist who promotes orthodontic treatments to correct malocclusions (incorrect forms of dental closure and articulation of the teeth).
In Portugal, the orthodontic specialty was officially recognized in 1999. For this reason, it is recommended that those who need orthodontic treatment should first be informed if the dentist they are going to consult is a specialist in orthodontics.
At Ortopóvoa, the Clinical Director, Prof. Dr. Afonso Pinhão Ferreira is a Dentist and Specialist in Orthodontics since 1999.
For further information, you can call the Portuguese Dental Association (22 6197690/21 7941344), the Dentofacial and Orthopaedics Portuguese Society (SPODF – 22 6099086) or the Portuguese Association of Orthodontists (APO – direcao.apo@gmail.com).
When is orthodontic treatment necessary?
Orthodontic treatment is necessary when there are malposition’s of the teeth and jaws (malocclusions) as well as functional problems in the buccal and facial structures.
Therefore, a treatment performed by an orthodontist should promote the following aims:


- To achieve a more harmonious face and an attractive smile, which usually results in the increase of the patient’s self-esteem with consequent ease of social insertion;
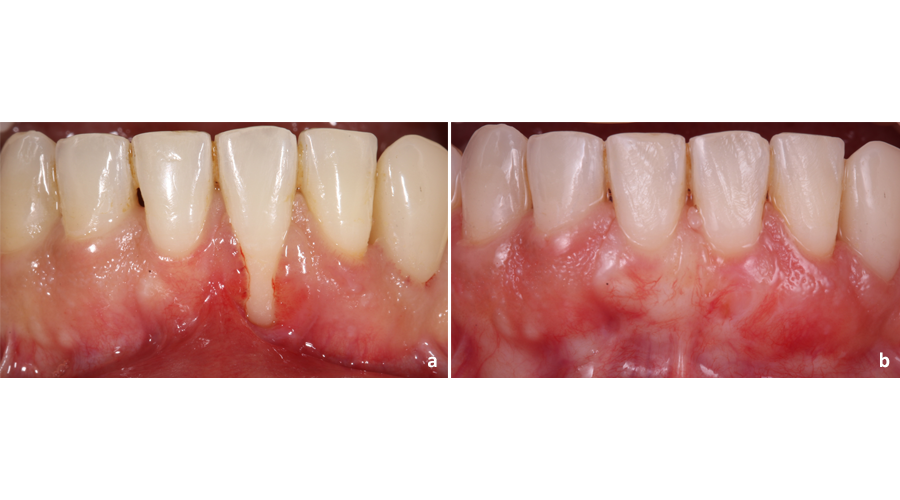
- To facilitate oral hygiene, which will result in reducing future dental and gums problems and increasing dental longevity. The following image shows the differences in the health status of the gums before and after orthodontic treatment;
- Reduce the probability of dental fractures, especially when teeth are positioned far ahead (protrusion);
- Improve mouth and adjacent structures functions (chewing and swallowing, breathing, speech and facial expression);
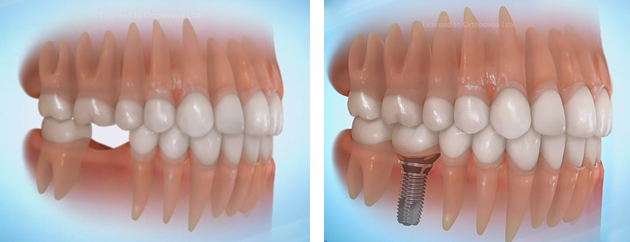
- Align teeth and where possible the jaws, restoring the proper function of the buccal structures, which will help dentists and other specialists to achieve better clinical outcomes in dental treatments, periodontal treatments, implant rehabilitation treatments and placement of fixed and / or removable prostheses;
- Prevent certain problems in the temporomandibular joints (joints that connect the mandible to the skull).
What are the main causes of orthodontic anomalies?
Orthodontic anomalies, such as malocclusions, may arise from hereditary or environmental causes or a combination of both. In fact, the dimension of the teeth and jaws as well as the relation between them, are features that can be transmitted from parents to children. To exemplify a hereditary factor, imagine a child who “inherits” the father’s large teeth and the mother’s small jaws. In this case, the teeth will not fit in the jaws, and therefore, they become misaligned (crowding).
Environmental factors are usually a consequence of harmful habits such as breathing through the mouth, sucking fingers and tongue, gnawing nails or other objects (such as pens). These habits can lead to incorrect tooth movements and changes in shape and position of the jaws, thus negatively affecting the facial harmony.
Another circumstance that can cause orthodontic anomalies is the premature loss of temporary/deciduous teeth due to dental caries. This is due to the fact that temporary teeth maintain the necessary space for the eruption of permanent teeth.
If a temporary tooth is lost, the adjacent teeth move into the created space and “steal” some of that area. When it is time to erupt the permanent teeth there will not be enough space, which will result in crowding and/or other similar problems.
The malocclusions
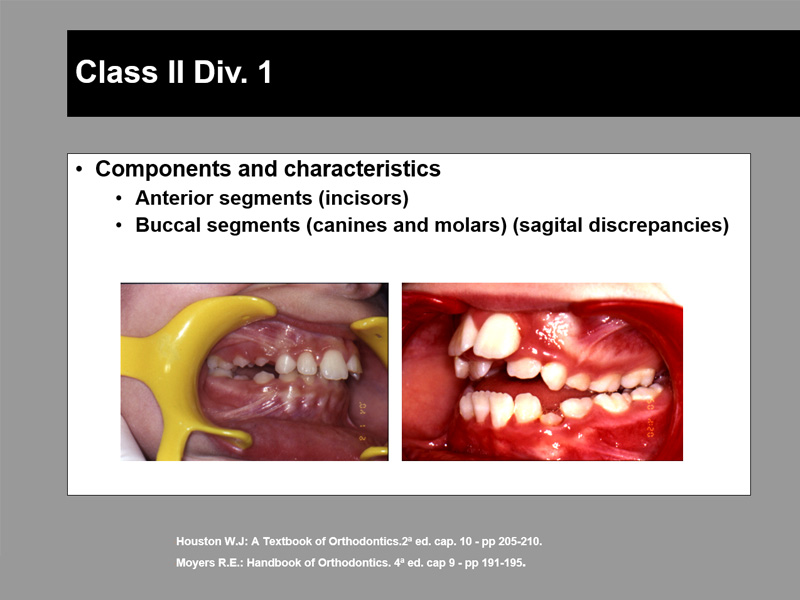
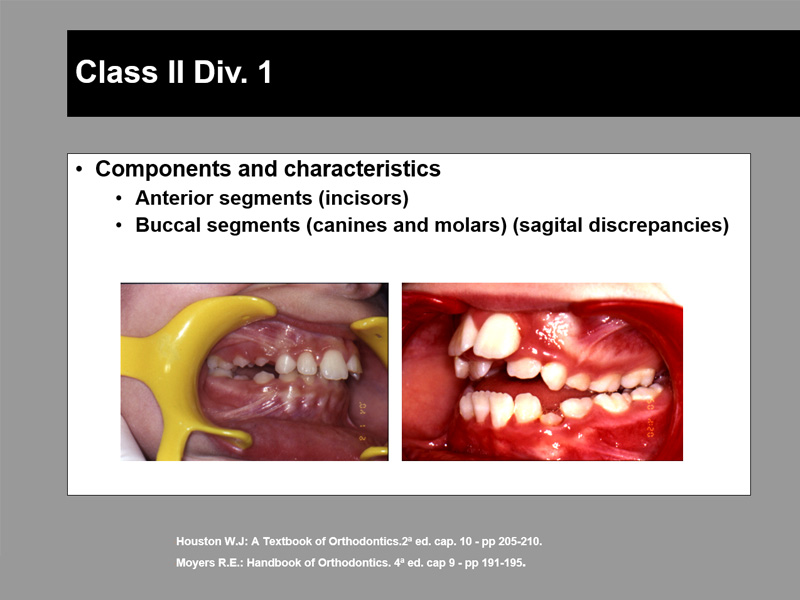
There are three categories of malocclusions usually treated by orthodontists:
In this first category, for the most varied reasons, the teeth are not placed correctly in the maxillary bones and, therefore, they appear to be misaligned (crowded or spaced). In these cases, the goal of orthodontic treatment is to correct the dental positions (orthodontics).
In the second category, the maxillary bones do not develop harmoniously, which represents a negative effect on facial aesthetics and oral functions. In these cases, the goal of orthodontic treatment is to promote facial harmony (dentofacial orthopaedics).
Here, there is a combination of dental and skeletal problems, affecting not only the oral cavity but also the aesthetics of the face. In these cases, the goal of the orthodontic treatment is to correct the position of the teeth and promote the balance of the face.
The orthodontic appliances
The appliances used during the orthodontic treatment may be removable, i.e., may be removed and placed by patients, or may be fixed, i.e., permanently attached to the teeth during the treatment period, and may only be removed by an orthodontist.
There is usually a slight discomfort in the first few days after the appliance is placed.

What kind of appliances are there?

Transversal expansion appliances are used to transversally enlarge the upper jaw and teeth. They are used to alter the shape of the dental arch.
In this category one includes the removable expansion devices that need to stay in the mouth for 24 hours/day and also the fixed expansion devices.

They are removable or fixed devices that can be used to correct maxillary bone discrepancies.
They are used when the orthodontist intends to orientate, stimulate or inhibit the development.
They are placed in very young children and are mainly used in pre-puberty or puberty.
The removable functional devices are mostly used during the night and for a few hours of the day.
The advantages of removable devices are the ease with which they can be cleaned and removed during meals. However, in patients where there is little or no cooperation during treatment, the fact that these devices can be removed may be a disadvantage, and therefore the fixed devices are more indicated.

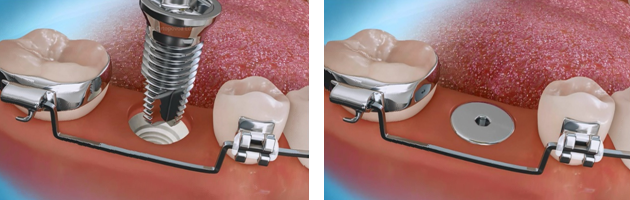
These are devices that develop forces capable of modifying the growth of the maxillary bones and can also be used to move the teeth into better positions.
In certain situations they can be used as a counterforce in order to prevent certain teeth from moving.
The headgear is the most common and consists of a facial bow and a elastic strap applied to the neck or head.
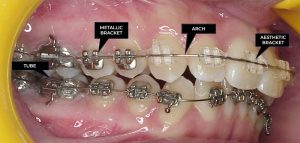
There are numerous devices that are used combining fixed appliances with different aims. Among these we can mention, the elastics, the elastic chains or certain special springs.
These devices, combined with the arches inserted in the slots of the brackets, cause forces that move the teeth in the three planes of space. They are used whenever it is necessary to move the teeth more accurately.

Once the orthodontic treatment (treatment’s active phase) is achieved, it is utterly necessary to maintain the outcome (treatment’s passive phase), since during a certain period of time there will be a tendency for the teeth to move to the previous positions (relapse).
The maintenance of the result, known as the retainer phase, is carried out with removable or permanent devices. The patient’s cooperation is crucial during this phase in order to avoid relapse, thereby ensuring the stability of the outcomes of the active treatment over time.
Orthodontic treatment in adults
The importance of orthodontist cooperation with other dental specialties
Patients with orthodontic problems who were not seen in a younger age may benefit from orthodontic treatment in adulthood.
In most cases, the treatment of adults requires the orthodontist cooperation with other specialties in dentistry or medicine (dentist, periodontist, oral surgeon, implantologist and prosthodontist, endodontist, plastic surgeon, maxillofacial surgeon, etc.).
These treatments can ensure the best functional and aesthetic result and indicate an advantage for the patient since he/she benefits from the treatment capabilities of the different specialties.
Orthodontic-surgical treatment
In certain cases of severe malocclusions, in addition to the orthodontic correction may be necessary surgical intervention.
The anomaly is so severe that if we move the teeth orthodontically to reach occlusion, they would leave the maxillary bones.
In fact, the maxillary bones themselves have disharmonious dimensions and positions. These anomalies are called dento-facial deformities (DDF).
To treat DDF, an interdisciplinary treatment called orthodontic-surgical is required.
In ORTOPÓVOA, these treatments are performed by the orthodontist, Prof. Dr. Afonso Pinhão Ferreira and the maxillofacial surgeon, Dr. Adriano Figueiredo, with the technical support of Ortopóvoa laboratory.
This complex and interdisciplinary treatment usually consists of three phases:
- An orthodontic preparation before surgery, where the teeth of each dental arch are independently aligned and levelled, in view of occlusal congruence during corrective surgery of the dimensions and discrepant positions of the maxillary bones (orthognathic surgery);
- Orthognathic surgery;
- A finishing orthodontic refinement.
The surgical-orthodontic treament is one of the most rewarding treatments from the occlusal rehabilitation and improvement of dentofacial aesthetics point of view.
It is now a routine procedure where the technology and clinical experience allow, without any scar, an amazing facial, jaws and teeth change, extremely rewarding for the patient with regard to their capacity for relational influence and self-esteem.

Orthodontic-surgical treatment

Orthodontic-surgical treatment
Patient-oriented management
Ortopóvoa believes in a patient-oriented management. Thus, we pay close attention to the patient’s main complaint and perform personalized care. For this reason, and despite many requests, we never considered feasible to open branches, as we would not be able to maintain the same quality.
Follow us on an orthodontic treatment.

- In the first appointment, you should go to the reception where you will be welcomed by Liliana, who will fill out your identification file and accompany you to the presence of the Administrative Director and Patient Coordinator Dr. Maria Alexandrina.
- You will then be taken to collect the necessary data for studying your clinical case. The assistant Carina will make intra- and extra-oral photographs, 3D scanning of buccal structures, panoramic radiography and lateral cephalometric radiography.
- Finally, and to complete the process of data collection, will be examined by the Clinical Director and Specialist in Orthodontics, Prof. Dr. Afonso Pinhão Ferreira.
- Next, the clinical staff will study the case, considering the diagnosis, the treatment plan, the time needed for its effectiveness, the prognosis and the budget.
- At the reception desk, you should schedule a new appointment to be informed of the results of the clinical study, the recommended orthodontic treatment and its budget.

This appointment is very interesting because the patient is totally informed about the overall aspects related to his/her case.
We believe that a good decision is based on wide-ranging information. Therefore, we advise the patient to join us with his/her family and/or friends. The appointment takes place in two different parts always with the help of audio-visual media. In the first part, the patient is informed about the bureaucratic aspects, such as:
- How Ortopóvoa works;
- How the clinical cases are studied;
- How the appliances are placed;
- How long takes the expected treatment;
- What is the budget and which are the payment possibilities.
In the second part, Prof. Dr. Afonso Pinhão Ferreira, clarifies the clinical features of the case by showing similar treated cases.
At the end of the consultation, a PDF document is sent to the patiens’s e-mail with all the diagnostic data as well as a written report where the treatment plan and the budget are listed. This document is accompanied by a term of responsibility which is stamped, identified, dated and signed.

After accepting the treatment proposal, the patient will be prepared for placing the orthodontic appliances.
Previously it may be necessary to:
- Do some periodontal treatment;
- Treat or extract some teeth;
- Make impressions to execute certain types of orthodontic devices;
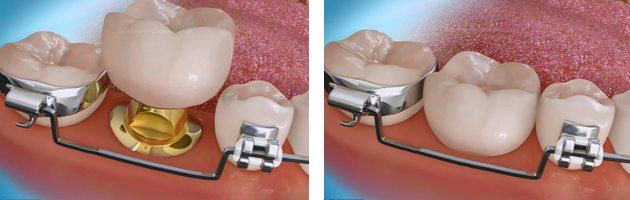
- Or simply place stainless steel bands to facilitate the placement of fixed appliances (this may be performed during the second appointment).

In this appointment we start the active phase of the orthodontic treatment.
We place and activate the devices and provide instructions for its use, especially with regard to oral hygiene care.
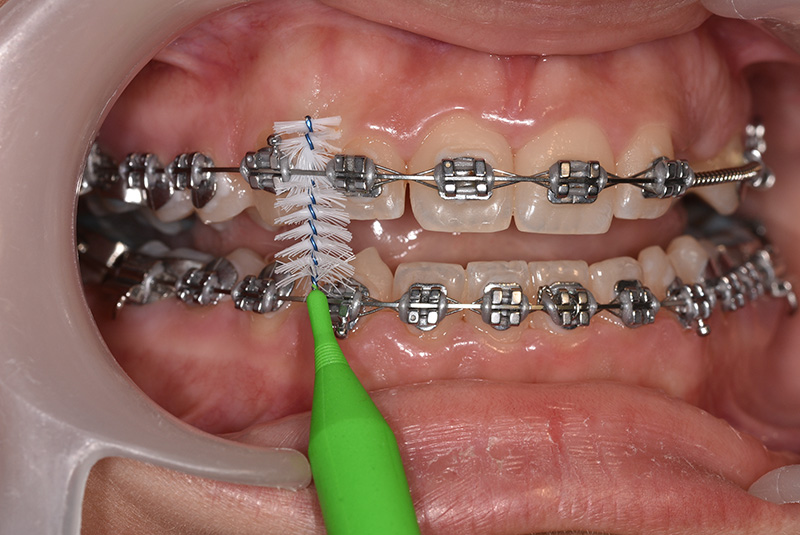
In the first few days, Ortopóvoa offers an orthodontic kit consisting of: a toothbrush, toothpaste, a mouthwash, protective wax and an interdental brush.
The patient or his/her caregivers must sign an informed consent, explaining in detail the advantages and disadvantages of the treatment (both parties keep a copy of this document).
Then the 1st control and activation of the devices (about a month to a month and a half) must be scheduled.

In the following appointments (usually monthly), we will monitor the evolution of treatment with:
- Activation of the appliances;
- Placement of auxiliary devices (headgear, intermaxillary elastics, etc.);
- Repair of appliances when necessary;
- Control and motivation of oral hygiene;
- Taking intra-oral photographs to record the clinical evolution of the case;
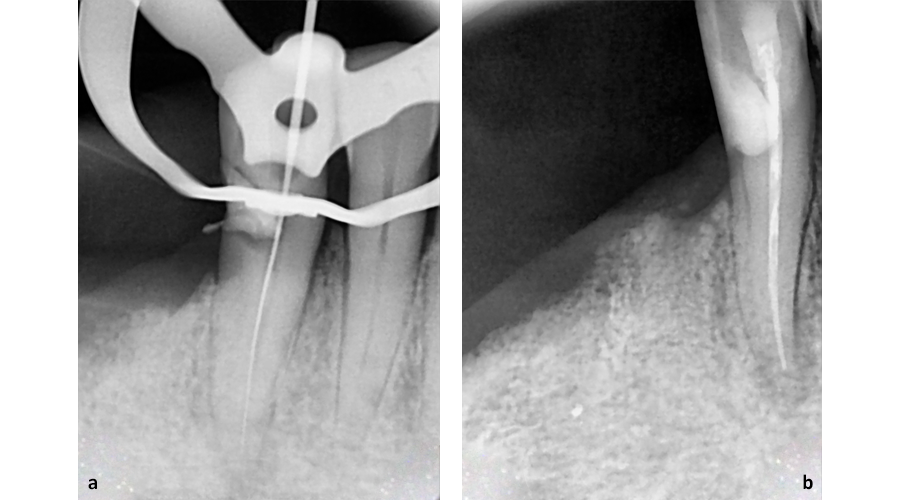
- Annual radiographic control;
- Information on treatment progress.
After achieving the aims of the orthodontic treatment and if the teeth are aligned and levelled, allowing functional occlusion, the devices are removed.
Thereafter, the dental arches are prepared for making retaining devices, i.e., orthodontic devices for night use during a period of time for preventing the teeth from misaligning and also to maintain treatment outcomes.
Usually happens one month after the removal of fixed appliances.
In this appointment:
- We control and adjust the retaining devices;
- We provide instructions on the use of the retainers and also their maintenance;
- We remind oral hygiene procedures;
- We collect x-rays and photographs to analyse and evaluate the treatment outcomes and also verify any treatment needs;
- We prepare a final report.
If there is no unforeseen event, the patient should schedule an appointment one year after finishing his orthodontic treatment.
This appointment is included in the budget.
Care
Before, during and after orthodontic treatment, there are numerous information and care to take into consideration, such as:
Children develop many habits that can cause dental and oral structural problems. Within these harmful habits we can point out mouth breathing (often related to large adenoids, asthmatic bronchitis, allergies, etc.), tension with teeth twitching, lingual pressure, biting and/or interposition of the lower lip, chewing fingernails or other objects (such as pencils, erasers, etc.), chewing only on one side, sucking fingers, etc.
In young children, the habit of sucking fingers usually stops between two and three years of age and the damage done is minor and can be solved without any special intervention. The children who, after that age, continue to exercise this habit can hide some kind of insecurity or stress caused by motives such as the absence of parents, moving home or even changing school.
In order to eradicate these problems, it’s important some support, affection and quality communication with the young ones. Even so, in more persistent cases, the orthodontist can support the parent’s effort by placing devices that help the child to overcome this habit. Yelling and punishing will surely be the worst possible approach. On the contrary, what will work best in these cases will be to encourage the children for the necessary effort and reward them when the goal is achieved.
During treatment we may need to extract some temporary teeth if they remain in the mouth beyond considered acceptable time. In some cases, the extraction or not of permanent teeth is a very thoughtful decision that the orthodontist must consider. Such situations occur when disproportion between the size of the jaws and the size of the teeth occurs (DMD – dento-maxillary disharmony) or when the skeletal development of the face is unbalanced (MMD – maxillomandibular disharmony). The orthodontist determines the timing for extraction and which teeth to extract, assuming the scientific and clinical responsibility for his decision.
The use of orthodontic appliances poses no risk to health, provided that they are applied by orthodontic specialists and that all recommended care is respected. One of the most important is undoubtedly the practice of a good oral hygiene.
Even so, the use of orthodontic appliances favours the retention of food and the development of bacterial plaque, which produces acids that will inflame the gums (swollen, red and bleeding) and demineralize the teeth (causing irreversible stains and caries). Therefore, it is important the inexistence of flaws in oral hygiene.
Our advice includes:
- Avoid eating or drinking sugary foods, and when you eat or drink, brush your teeth afterwards;
- Brush all the teeth (top and bottom, front and back, inside and out, without forgetting any, with small rotating movements) for two minutes counted by the clock, with a brush neither too hard nor too much soft (renewed every three months), after breakfast, after lunch and before going to bed;
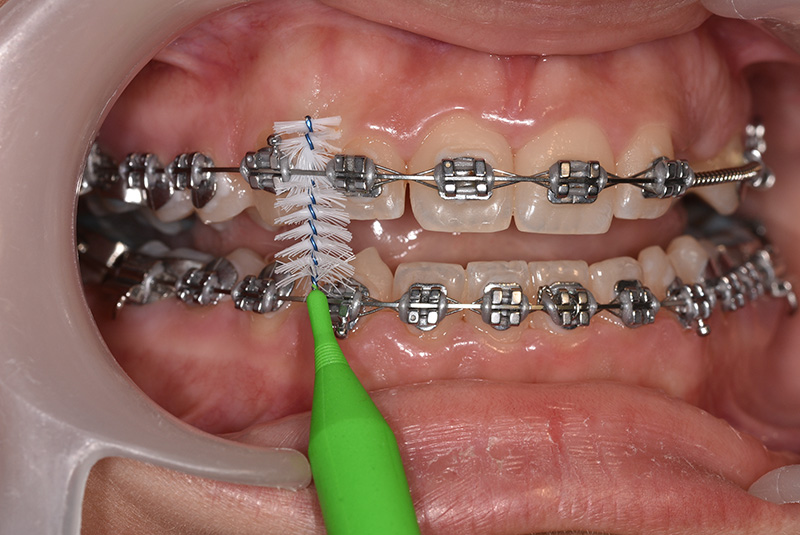
- We advise the use of an interdental brush, since it allows cleaning inaccessible places more than the usual brushing technique. In fact, the use of a small brush with back and forth movements inserted in the interdental spaces, between the brackets, the arches and the teeth, allows a careful cleaning of these places. Therefore, we recommend using the interdental brush before traditional brushing, at least once a day, preferably at night. Alternatively, you can use dental floss;
- Brush the tongue whenever you brush your teeth (it decreases the number of bacteria);
- Whenever you eat food in between tooth brushing, you must vigorously rinse three times with water (it reduces the number of food, bacteria and acids);
- Flushing with fluoridated mouthwash twice a day (morning and night).

The outcome of orthodontic treatments is determined by permanent forces carried out by appliances throughout time. In some cases it may be necessary some additional force to move the teeth into correct positions. This is why the orthodontist asks the patient to use elastics. If used according to the specialist’s instructions, the faster you will get a healthy and beautiful smile.
Intermaxillary elastics, when used correctly, can cause some discomfort, making the teeth sore for a day or two. When the elastics are not used according to the instructions of the orthodontist, this discomfort lasts even longer and the teeth take much longer to reach the desired position.
To accomplish a better outcome when using elastics:
- It is the patient’s responsibility to wear the elastics correctly and it is important to make sure that they are used regularly and according to the instructions;
- The patient should always carry some elastics in case of any bursting. This way the patient can replace them when needed. If one doesn’t have spare elastics, the patient should contact ORTOPÓVOA to request more;
- When the patient forgets to wear the elastics, which should not happen, he should use them normally as indicated, as soon as possible;
- Elastics lose strength over time, and when this happens, the teeth and jaws are not receiving the wanted pressure. Therefore, it is important to change elastics even when they are not broken;
- When brushing the teeth, the elastics should be removed and replaced soon afterwards and this should be done in front of a mirror.

The headgear and facebow are auxiliary devices that belongs to extra-oral appliances (devices that work forces inside the mouth with anchoring outside the mouth).
It is an orthopaedic device that develops forces in order to alter the growth of the face and maxillary bones. It is also used to move the teeth to better positions or to prevent them from moving when necessary.
This extra-oral device consists of a facebow and a headgear with a safety device. The inner arch of the facial bow is inserted into the attachments soldered to the bands (tubes), cemented around the first molars (small metal rings).
The facebow should be used on a daily basis according to the instructions (even on birthday and Christmas day), under the risk of being very difficult to overcome the barriers that the body creates to the displacement of bones. Every single day the device is not used, it implies a week of delay in treatment.
It should be placed and removed according to the instructions to avoid injury, even though the appliance has a safety device.
Whenever the patient goes to the control appointment, he or she should take the facebow, and if there is any problem (such as a loose band or if the appliance hurts), the patient should contact ORTOPÓVOA.
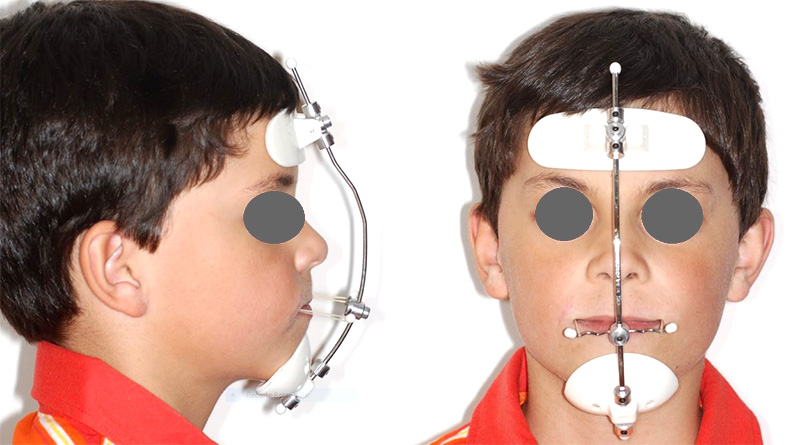
The face mask is an auxiliary device that belongs to extra-oral appliances (devices that work forces inside the mouth with anchoring outside the mouth).
It is an orthopaedic device that develops forces in order to alter the growth of the face and maxillary bones. The facial mask is used to move forward the upper jaw and the teeth into better positions.
The face mask should be worn every day according to the instructions (even on birthday and Christmas day), under the risk of overcoming the barriers that the body creates to bone displacement. Each day the patient doesn’t use the face mask, it implies a week of delay in the treatment.
Whenever the patient goes to the control appointment, he or she should take the face mask, and if there is any problem (such as a loose band or if the appliance hurts), the patient should contact ORTOPÓVOA.
Devices used during orthodontic treatment may be removable (removed and placed by the patient), or fixed (permanently attached to the teeth during the treatment period and can only be removed by the orthodontist).
There are several types of removable appliances, of which we highlight the most used:
- Biomechanical devices (known as active plaques);
- Functional devices (Bionator, Bimler, Frankell, Andresen’s Monobloc, etc.);
- Retainer devices (Hawley plaque, Essix retainers, etc.).

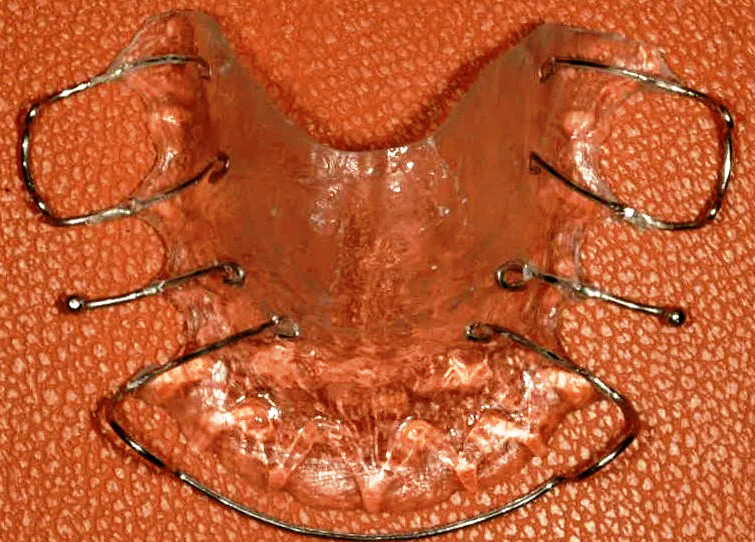
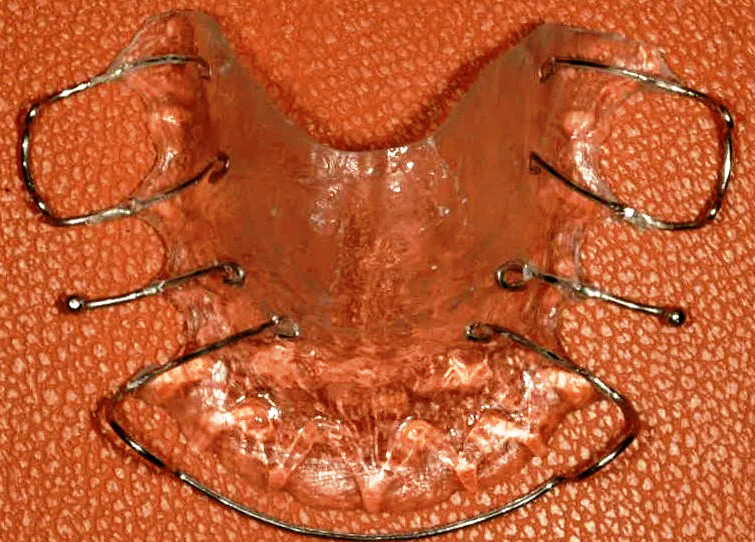
Biomechanical devices consist of two components:
- An acrylic portion that covers the palate in the case of the upper jaw;
- Metal components (bows, hooks and springs) attached in the acrylic which serve to promote retention in the mouth and to develop forces to move the teeth.
The removable functional appliances are used to correct dimensions and positions of the maxillary bones. They are placed in young children and used in pre-puberty or puberty.
Removable functional devices are used all day long.

These devices take advantage of the functionality of the mouth to develop forces with more suited vectors to face growth. For example, when the patient swallows the saliva (which he does 60 times per hour), he is forced to close his teeth and, if he is using the functional appliance, this closure will be oriented to a more favourable position for the growth and positioning of the mandible.
After removing the fixed appliance to prevent the teeth from returning to their positions before treatment, it is important to keep them in the correct final position, especially in the first few years after orthodontic treatment.
The role of this type of device is to prevent relapse, that is, to prevent the teeth from returning to undesirable positions.
For this purpose, there are retainers, mainly for night use.
There are also retainer splints for the same effect consisting of a wire bonded or fixed in the lingual surfaces of the anterior teeth, keeping them “united”, thus avoiding their displacement.
The most commonly used removable retaining device is called Hawley Retainer. It consists of an acrylic plaque, retaining hooks and a vestibular arch.
These three components cooperate to maintain the final position of the teeth.
Children develop many habits that can cause dental and oral structural problems. Within these harmful habits we can point out mouth breathing (often related to large adenoids, asthmatic bronchitis, allergies, etc.), tension with teeth twitching, lingual pressure, biting and/or interposition of the lower lip, chewing fingernails or other objects (such as pencils, erasers, etc.), chewing only on one side, sucking fingers, etc.
In young children, the habit of sucking fingers usually stops between two and three years of age and the damage done is minor and can be solved without any special intervention. The children who, after that age, continue to exercise this habit can hide some kind of insecurity or stress caused by motives such as the absence of parents, moving home or even changing school.
In order to eradicate these problems, it’s important some support, affection and quality communication with the young ones. Even so, in more persistent cases, the orthodontist can support the parent’s effort by placing devices that help the child to overcome this habit. Yelling and punishing will surely be the worst possible approach. On the contrary, what will work best in these cases will be to encourage the children for the necessary effort and reward them when the goal is achieved.
During treatment we may need to extract some temporary teeth if they remain in the mouth beyond considered acceptable time. In some cases, the extraction or not of permanent teeth is a very thoughtful decision that the orthodontist must consider. Such situations occur when disproportion between the size of the jaws and the size of the teeth occurs (DMD – dento-maxillary disharmony) or when the skeletal development of the face is unbalanced (MMD – maxillomandibular disharmony). The orthodontist determines the timing for extraction and which teeth to extract, assuming the scientific and clinical responsibility for his decision.
The use of orthodontic appliances poses no risk to health, provided that they are applied by orthodontic specialists and that all recommended care is respected. One of the most important is undoubtedly the practice of a good oral hygiene.
Even so, the use of orthodontic appliances favours the retention of food and the development of bacterial plaque, which produces acids that will inflame the gums (swollen, red and bleeding) and demineralize the teeth (causing irreversible stains and caries). Therefore, it is important the inexistence of flaws in oral hygiene.
Our advice includes:
- Avoid eating or drinking sugary foods, and when you eat or drink, brush your teeth afterwards;
- Brush all the teeth (top and bottom, front and back, inside and out, without forgetting any, with small rotating movements) for two minutes counted by the clock, with a brush neither too hard nor too much soft (renewed every three months), after breakfast, after lunch and before going to bed;
- We advise the use of an interdental brush, since it allows cleaning inaccessible places more than the usual brushing technique. In fact, the use of a small brush with back and forth movements inserted in the interdental spaces, between the brackets, the arches and the teeth, allows a careful cleaning of these places. Therefore, we recommend using the interdental brush before traditional brushing, at least once a day, preferably at night. Alternatively, you can use dental floss;
- Brush the tongue whenever you brush your teeth (it decreases the number of bacteria);
- Whenever you eat food in between tooth brushing, you must vigorously rinse three times with water (it reduces the number of food, bacteria and acids);
- Flushing with fluoridated mouthwash twice a day (morning and night).

The outcome of orthodontic treatments is determined by permanent forces carried out by appliances throughout time. In some cases it may be necessary some additional force to move the teeth into correct positions. This is why the orthodontist asks the patient to use elastics. If used according to the specialist’s instructions, the faster you will get a healthy and beautiful smile.
Intermaxillary elastics, when used correctly, can cause some discomfort, making the teeth sore for a day or two. When the elastics are not used according to the instructions of the orthodontist, this discomfort lasts even longer and the teeth take much longer to reach the desired position.
To accomplish a better outcome when using elastics:
- It is the patient’s responsibility to wear the elastics correctly and it is important to make sure that they are used regularly and according to the instructions;
- The patient should always carry some elastics in case of any bursting. This way the patient can replace them when needed. If one doesn’t have spare elastics, the patient should contact ORTOPÓVOA to request more;
- When the patient forgets to wear the elastics, which should not happen, he should use them normally as indicated, as soon as possible;
- Elastics lose strength over time, and when this happens, the teeth and jaws are not receiving the wanted pressure. Therefore, it is important to change elastics even when they are not broken;
- When brushing the teeth, the elastics should be removed and replaced soon afterwards and this should be done in front of a mirror.

The headgear and facebow are auxiliary devices that belongs to extra-oral appliances (devices that work forces inside the mouth with anchoring outside the mouth).
It is an orthopaedic device that develops forces in order to alter the growth of the face and maxillary bones. It is also used to move the teeth to better positions or to prevent them from moving when necessary.
This extra-oral device consists of a facebow and a headgear with a safety device. The inner arch of the facial bow is inserted into the attachments soldered to the bands (tubes), cemented around the first molars (small metal rings).
The facebow should be used on a daily basis according to the instructions (even on birthday and Christmas day), under the risk of being very difficult to overcome the barriers that the body creates to the displacement of bones. Every single day the device is not used, it implies a week of delay in treatment.
It should be placed and removed according to the instructions to avoid injury, even though the appliance has a safety device.
Whenever the patient goes to the control appointment, he or she should take the facebow, and if there is any problem (such as a loose band or if the appliance hurts), the patient should contact ORTOPÓVOA.
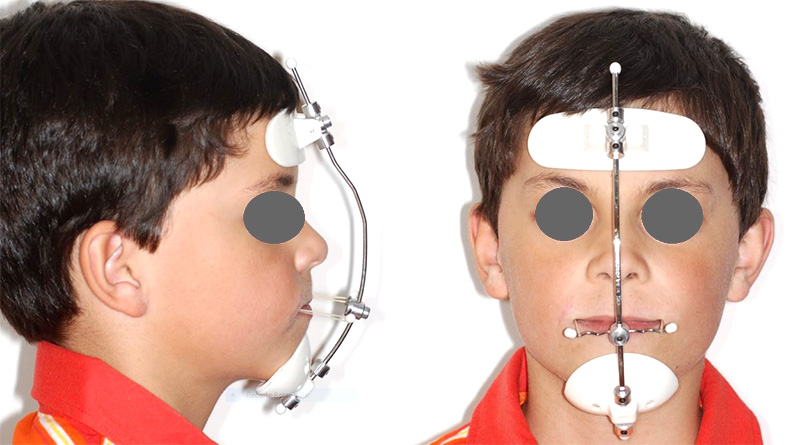
The face mask is an auxiliary device that belongs to extra-oral appliances (devices that work forces inside the mouth with anchoring outside the mouth).
It is an orthopaedic device that develops forces in order to alter the growth of the face and maxillary bones. The facial mask is used to move forward the upper jaw and the teeth into better positions.
The face mask should be worn every day according to the instructions (even on birthday and Christmas day), under the risk of overcoming the barriers that the body creates to bone displacement. Each day the patient doesn’t use the face mask, it implies a week of delay in the treatment.
Whenever the patient goes to the control appointment, he or she should take the face mask, and if there is any problem (such as a loose band or if the appliance hurts), the patient should contact ORTOPÓVOA.
Devices used during orthodontic treatment may be removable (removed and placed by the patient), or fixed (permanently attached to the teeth during the treatment period and can only be removed by the orthodontist).
There are several types of removable appliances, of which we highlight the most used:
- Biomechanical devices (known as active plaques);
- Functional devices (Bionator, Bimler, Frankell, Andresen’s Monobloc, etc.);
- Retainer devices (Hawley plaque, Essix retainers, etc.).

Biomechanical devices consist of two components:
- An acrylic portion that covers the palate in the case of the upper jaw;
- Metal components (bows, hooks and springs) attached in the acrylic which serve to promote retention in the mouth and to develop forces to move the teeth.
The removable functional appliances are used to correct dimensions and positions of the maxillary bones. They are placed in young children and used in pre-puberty or puberty.
Removable functional devices are used all day long.

These devices take advantage of the functionality of the mouth to develop forces with more suited vectors to face growth. For example, when the patient swallows the saliva (which he does 60 times per hour), he is forced to close his teeth and, if he is using the functional appliance, this closure will be oriented to a more favourable position for the growth and positioning of the mandible.
After removing the fixed appliance to prevent the teeth from returning to their positions before treatment, it is important to keep them in the correct final position, especially in the first few years after orthodontic treatment.
The role of this type of device is to prevent relapse, that is, to prevent the teeth from returning to undesirable positions.
For this purpose, there are retainers, mainly for night use.
There are also retainer splints for the same effect consisting of a wire bonded or fixed in the lingual surfaces of the anterior teeth, keeping them “united”, thus avoiding their displacement.
The most commonly used removable retaining device is called Hawley Retainer. It consists of an acrylic plaque, retaining hooks and a vestibular arch.
These three components cooperate to maintain the final position of the teeth.
Common questions
The sooner the better
Prevention is essential in any medical or dental specialty. For this reason, we recommend that the first visit to the orthodontist to be before the age of seven. It is the ideal time for the orthodontist to observe the patient, identify the problems, assess the severity and decide the best time to start orthodontic treatment.
Preventive orthodontics, targeted to very young patients, aims to treat some situations, such as premature loss of temporary teeth, prolonged finger sucking and incorrect tongue positions. In cases where finger sucking and tongue projection occurs, it is possible to interrupt these harmful habits without the use of orthodontic appliances provided that both parents and children are properly instructed and oriented.
The treatments carried out between seven and nine years old correspond to the so-called interceptive orthodontics. Its purpose is to promote treatments in order to avoid functional and skeletal problems.
If these problems are not promptly treated, they will allow an incorrect growth and development of the oral and facial structures.
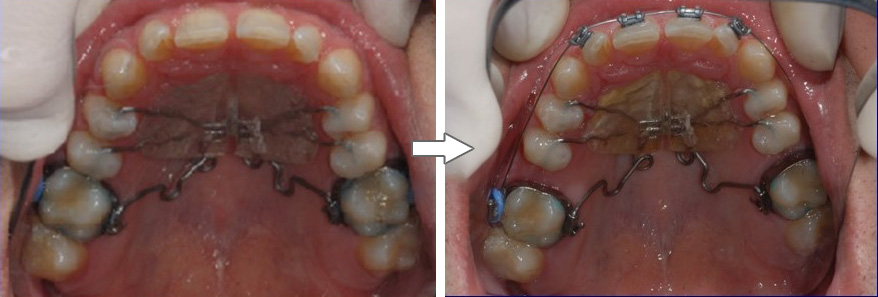
The following image shows the result of an interceptive treatment where an anterior crossbite was rectified. Corrective orthodontics treats completely established malocclusions in children or adults.

The ideal time to start a corrective treatment is determined by the orthodontist and it depends on the severity and the growth of the teeth and maxillary bones.
- Better prognosis for avoiding extraction of permanent teeth;
- Supervision and easier orientation of maxillary bone problems, since the orthodontist can control the skeletal development before the onset of puberty (dentofacial orthopaedics);
- Better reaction of biological tissues to treatment;
- Easier adaptation of young patients to appliances;
- Younger children are not apprehensive and generally do not have psychological problems such as adolescents;
- When treatment starts earlier it ends before the child enters puberty. For this reason, they have more self-esteem than other adolescents, since they have improved their facial aesthetics;
- Adult patients, whose bone development is completed, are most often subjected to permanent tooth extractions or, if they have severe skeletal problems, require orthognathic surgery (to correct maxillary bone dimensions and positions).